Asthma

People are looking for a way to make their lives better, for a way to make things easier. Find It Medical is aimed at making high quality products and information easily accessible in order to en...
Read more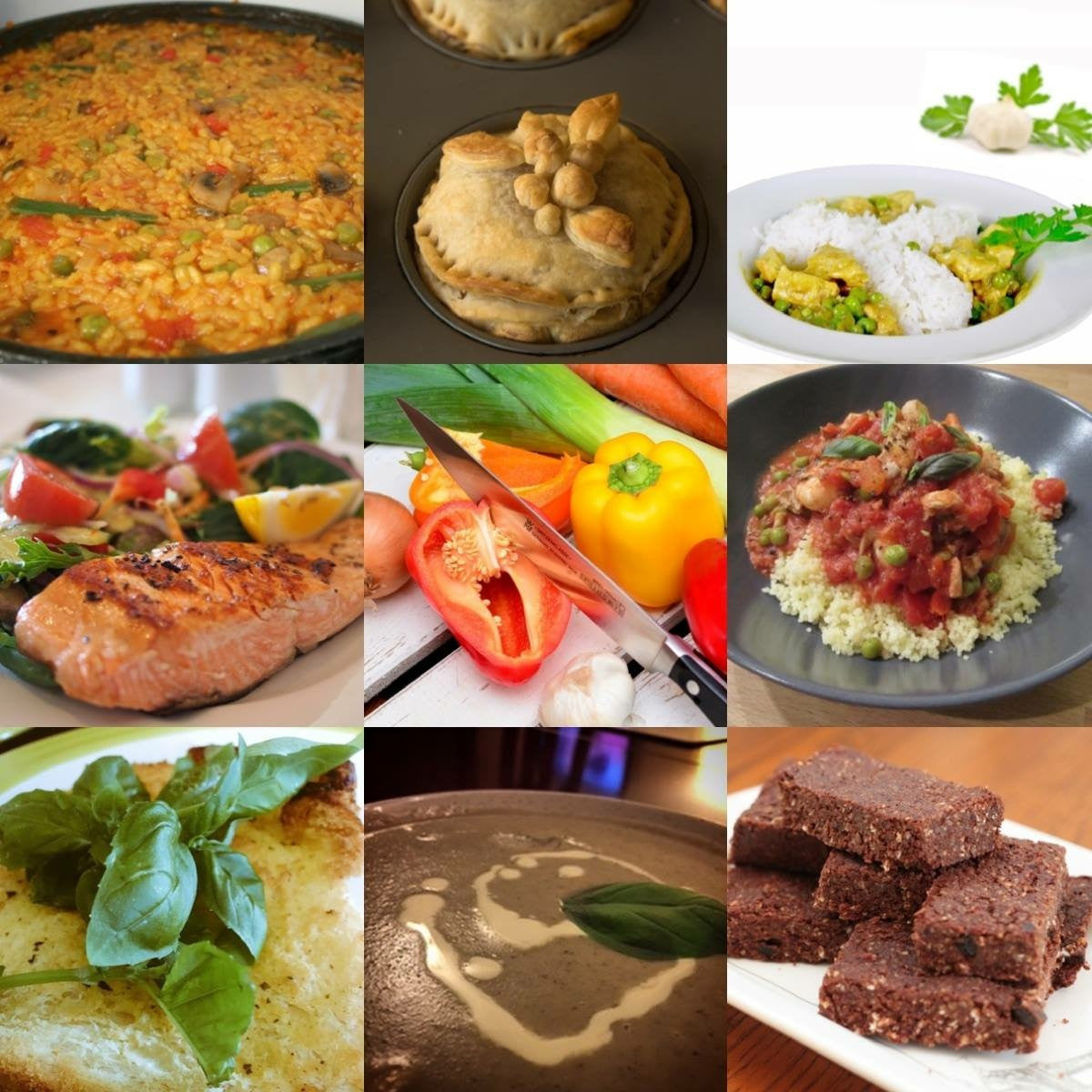
Hi I'm Marie, I'm a Nutritionist and PT, I run marathons, swim, lift weights, my passion is Thai boxing and I have Asthma, but certainly WONT stop me! - 300,000 million worldwide, Five million...
Read more
An Athlete’s Long Journey to Overcoming Asthma I’m a late-lift athlete, a female weight lifter, but not the kind that lifts super-heavy weights for one rep. I lift a moderate weight; 44lb or 53l...
Read moreGirl Recovering from Critical Asthma Attack Launches Foundation to Raise Awareness
Source: Miami Herald When Ashley Marie Hierrezuelo, 12, left her dance practice three months ago, she didn’t feel well and asked to go to the hospital. Her parents figured it was another asthma att...
Read moreWindsor Locks Police Officers Credited With Saving Boy Having Asthma attack
Chances are, you or someone you know has asthma. You may have even seen firsthand someone gasping for air while suffering an asthma attack. “The number of people with asthma continues to grow. One ...
Read moreI first got athletic induced asthma or so I thought when I was 28. I used to run 10-15 miles per day, back in the day. I'm in my mid 50's now. So I was put on Ventolin and life went on. In bad year...
Read more