Dementia
Reset the Age of your Stem Cells and Become Healthy Again
Stem cells are the resident cells in your tissues which divide and give rise to all of the specialized cells which constitute your organs. Your heart, brain, kidneys, pancreas, liver, and the rest ...
Read morePersonal Stories: Critterish Allsorts
I am involved in the Dementia community, as a complementary therapist. I visit care homes and sufferers in their own homes. I work in both group and one-to-one sessions helping dementia sufferers w...
Read moreStudy: Controlling Blood Sugar May Prevent Dementia
Controlling blood-sugar levels may help prevent dementia, a study released on Tuesday showed, offering hope to patients with diabetes that keeping glucose levels in check might reduce the risk of d...
Read moreHow do you explain Dementia to a child? Dementia can be scary, and children may wonder if the grandparent, or person suffering from Dementia, will remember them. Will Grandpa or Grandma see them? T...
Read moreHelping Dementia Patients with Music
Many years ago I developed a music calculating device called the MUSICULE™ “makes music easy” It is a Physical Product with corresponding theory Book written around the product for users to complet...
Read moreI was diagnosed with Young Onset Alzheimers on the 31 st July 2014. I used to be a very private person before diagnosed but was so shocked at the lack of awareness and understanding that I now sho...
Read more
Dementia can happen to anyone and there's currently no cure. There are 850,000 people with dementia in the UK and the number is set to rise to 1 million by 2021. At Alzheimer's Society, we believe...
Read moreInternational K-9 Search and Rescue Services
Hello, my name is Mr. Harry Oakes. I'm the K9 Search and Rescue Coordinator for International K9 Search and Rescue Services. We're on call 24/7 to respond anywhere in the world to search for missin...
Read more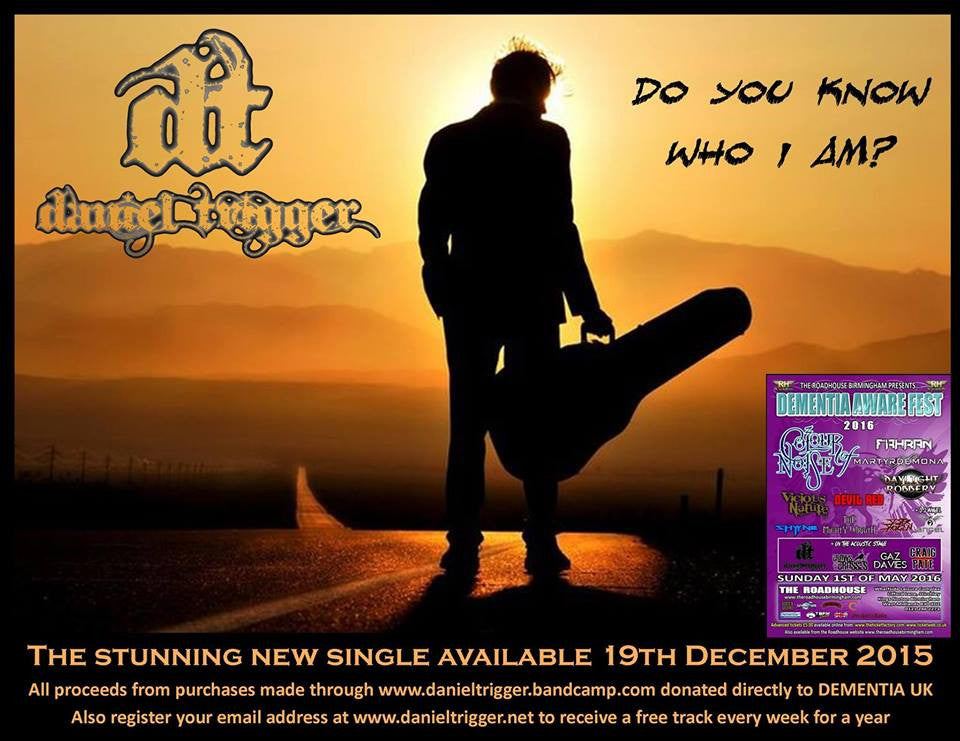
Daniel Trigger is generously donating all the proceeds from sales of his music at www.danieltrigger.bandcamp.com/ directly to Dementia UK, and who is also headlining the acoustic stage of the Demen...
Read moreUK Rockstar Donates Proceeds to Dementia Charity!
New single from UK singer/songwriter Daniel Trigger. Important - ALL proceeds from purchases of this track made through www.danieltrigger.bandcamp.com will be directed to the Dementia UK charity...
Read more